Over 30 million individuals in america reside with diabetes, and roughly 7.7 million individuals have diabetic retinopathy, making it the commonest reason behind vision loss in working-aged adults. The prevalence of diabetic retinopathy has elevated considerably over the previous 20 years, because of the rise within the variety of individuals identified with diabetes.
How does diabetes have an effect on the retina?
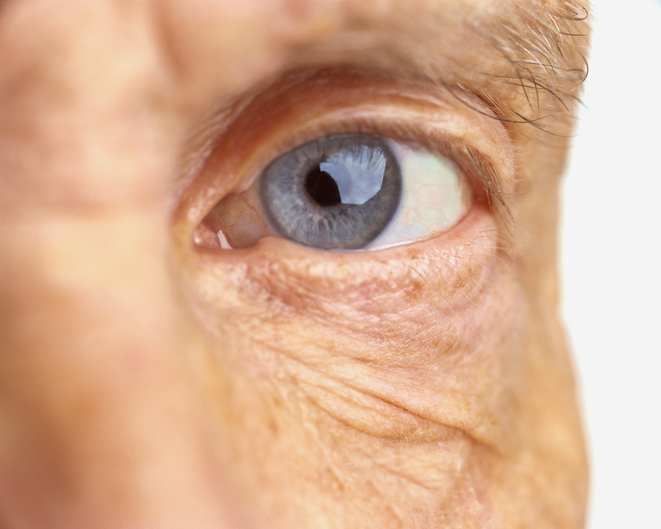
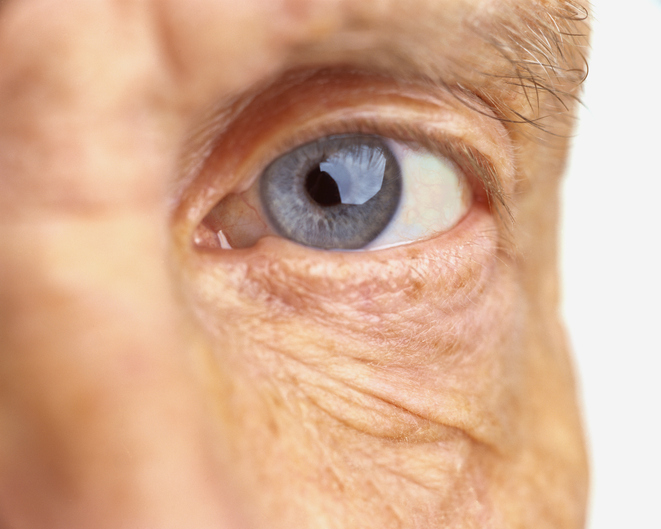
The retina is the sunshine-sensing element situated behind the eye. It’s composed of blood vessels, nerve cells (neurons), and specialised cells referred to as photoreceptors which are concerned in straight sensing gentle. The power of the retina to sense gentle requires power, which depends on the oxygen provided by blood circulating via blood vessels.
In diabetes, elevated blood sugar ranges injury the blood vessels of the retina. These broken blood vessels leak fluid, bleed, and don’t present sufficient oxygen to the retina, resulting in retinal ischemia. Consequently, retinal cells start to die and the retina is unable to operate correctly. As well as, diabetes additionally damages the neurons of the retina straight. Collectively, these results trigger diabetic retinopathy.
Vision loss related to diabetic retinopathy might initially have an effect on central vision as a consequence of a situation referred to as diabetic macular edema. This swelling of the macula, a portion of the retina chargeable for sharp, central vision, can result in blurry vision and distortion of photographs.
Superior diabetic retinopathy is characterised by the formation of irregular blood vessels that may bleed contained in the eye, inflicting a speedy loss of vision. This leads to a sudden, curtain-like vision loss as blood fills up the within of the eye. Additional worsening of superior diabetic retinopathy can result in retinal detachment, which requires pressing surgical intervention and may end up in everlasting, irreversible vision loss if not promptly handled.
What can I do to stop diabetic retinopathy?
The American Diabetes Affiliation recommends that most individuals with diabetes hold their A1c degree (a measure of common blood sugar ranges over the earlier two to a few months) beneath 7% to stop the danger of issues. As blood glucose straight damages retinal blood vessels, there’s sturdy epidemiological proof that blood sugar management interprets to decreased incidence and severity of diabetic retinopathy.
With a view to cut back the cardiovascular and microvascular issues of diabetes, which embrace retinopathy, nephropathy (kidney disease), and neuropathy (nerve injury), it’s endorsed that individuals obtain and keep a standard blood stress. Blood stress discount can delay the onset of diabetic retinopathy, however it’s unclear if controlling blood stress can alter the course of established diabetic retinopathy. Equally, managing ldl cholesterol is advocated for general diabetes administration, however it isn’t clear whether or not doing so reduces the danger of diabetic retinopathy.
How can I discover out if I’ve diabetic retinopathy?
An ophthalmologist can diagnose and start to deal with diabetic retinopathy earlier than sight is affected. Normally, individuals with sort 1 diabetes ought to see an ophthalmologist yearly, starting 5 years after the onset of their disease. Folks with sort 2 diabetes ought to see an ophthalmologist for a retinal examination quickly after their prognosis, and then schedule annual exams after that. You might must see an ophthalmologist extra incessantly if you’re pregnant or have extra superior diabetic retinopathy.
What can I do to stop or decelerate vision loss if I’ve diabetic retinopathy?
As talked about above, injury to the blood vessels deprives the retina of oxygen. Inadequate oxygen results in manufacturing of a sign protein referred to as vascular endothelial progress issue (VEGF). VEGF and its position in eye disease had been first found at Harvard Medical College.
At present, there are medicines that may bind VEGF and subsequently enhance the signs of diabetic retinopathy. These “anti-VEGF” brokers are injected straight into the eye and can enhance diabetic macular edema, and may even enhance the severity of diabetic retinopathy. In some individuals, steroids injected straight into the eye might also enhance diabetic macular edema. In some superior circumstances of proliferative diabetic retinopathy (probably the most superior type of diabetic retinopathy), sufferers might require retinal laser remedy or retinal surgical procedure to cease or gradual bleeding and leakage, to shrink broken blood vessels, or to take away blood and scar tissue.